48 hours
It was a long 48 hours – 48 hours that saw my grandfather step to the brink of death and back again. The good news – he’s alive and doing (relatively) well. But it was a roller coaster ride that started on Tuesday evening.
Tuesday Night
I was coming home from the iRise training and stopped by my grandfather’s store to see him. When I got there, I found out that he was at Riddle Memorial Hospital in Media. His partner thought it had to do with low blood pressure from not eating or drinking very well, plus a few other unsavory symptoms. I got to the hospital and found out he was in the ER, although that turned out to be only because they didn’t have any bed available. I talked to my uncle and he gave me the whole story – grandpop hadn’t been eating for 3 days and was complaining about back pain; when he doctor saw him, he thought he looked terrible and wanted him in for some tests.
He did look terrible – weak, tired and barely speaking. Michael and I stayed there for a while as the nurses did tests and made him comfortable. Eventually, he wanted to eat and I got him a sandwich. After some IV fluids and a sandwich, he actually looked pretty good when we left him to sleep. We figured he would be discharged the next day.
Wednesday Afternoon
After getting out of my training, I got back to the office, went to a couple of meetings and then made a call to my uncle’s to check on my grandfather. That’s when I got the news – he had a thoracic aneurysm and was in dire straits. Details were sketchy, particularly going between my two uncles who each had half of the story and my father, who had less than that. But what I did know was that it was life-threatening and Riddle Hospital couldn’t do the surgery necessary; they were waiting for a bed to open up at UPenn Hospital and they were going to rush him over there.
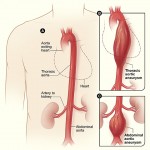 I called Shari to let her know I was coming home and would pick her up to go to the hospital. But we soon found ourselves in a state of limbo – they were waiting for the bed, and he might leave at any time. We could head to Riddle, but might find out that he had already been sent to Penn; we could wait for him to head to Penn, but that might not be for hours. But we did get more information – according to Riddle (which would become a sticking point), he had a 6cm thoracic aortic aneurysm¹, something that my great-uncle (who is a cardiovascular expert) said would probably kill him in 24 hours if he didn’t have surgery. Problem was, with his other conditions, surgery might not be an option.
I called Shari to let her know I was coming home and would pick her up to go to the hospital. But we soon found ourselves in a state of limbo – they were waiting for the bed, and he might leave at any time. We could head to Riddle, but might find out that he had already been sent to Penn; we could wait for him to head to Penn, but that might not be for hours. But we did get more information – according to Riddle (which would become a sticking point), he had a 6cm thoracic aortic aneurysm¹, something that my great-uncle (who is a cardiovascular expert) said would probably kill him in 24 hours if he didn’t have surgery. Problem was, with his other conditions, surgery might not be an option.
So, we waited … and waited. There was no word all night, but I figured no news was good news, although I had my cell phone by the bed, just in case.
Thursday Morning
Thursday morning, we learned that he had been moved to UPenn overnight and was in their Cardiothoracic ICU. They were going to do their own tests, and we would know more around noon. Things were grim, and seeing as how I couldn’t do anything at home except wait around, I went to work for a couple of hours. I then trekked up to UPenn to see him.
I was the first one there, and he didn’t look good. The nurses said that he was stable and comfortable, but they really couldn’t tell us much more. He was sleeping and would actually spend most of his time asleep except when they had to do something with him. He seemed cognizant of who we were but it was hard to tell if he truly knew what was going on around him. He had an NG tube (nasogastric?) to reduce his hiatal hernia (which could present complications) and so he couldn’t speak well anyway, but even considering that he seemed to be mumbling and nearly unintelligible. It was tough to watch. But at least he was being pleasant, something that the nurses at Riddle would attest that he was not during his final hours there (it seems that the low BP was causing some dementia-like symptoms).
As time went by, my cousins Marianne and uncle Joey showed up. We talked to grandpop and tried to keep him interactive, but he kept lolling off to sleep and seeming less and less lucid. The worry was palpable in the room as they did more tests, and we all were making calls to other relatives letting them know that we were still waiting for the test results. But we were getting worried – my great-uncle had said that he wouldn’t last 24 hours without surgery and we were rapidly approaching that mark.
Thursday Afternoon
At about 4:30, the attending on the floor finally came by with some results for us – and they weren’t good. He told us that there was indeed an aneurysm but that it not only was in the ascending aorta (more serious than the descending or thoracic area) and was also involving the aortic arch – the series of large arteries that lead directly to the brain. He said that surgery was simply not an option, as it would be a very complex operation involving a heart-lung bypass and actually stopping the heart to replace the aortic arch. The surgery would most likely be fatal either directly or within a couple of weeks, all of which would probably be spent on a respirator in the hospital. He was better off simply treating it – but he couldn’t (or wouldn’t, understandably) give us the odds of his survival without the surgery, only that they were better than heading to an OR. I had done some research (as I always do) and everything he said was bad – very bad. It looked like time had almost run out. All that remained was to talk to the cardiac surgeon to get the final word.
The calls went out – I called my sister and my father; Joey called my aunts and uncles. Shari, who had been waiting to hear what was happening, left to join us. I talked to my friend Rosemary, who works at UPenn, and she said that she would look up the doctor and let us know what she could, although it might be a moot point. My father was rushing up from N.C. and my sister started asking if she needed to make arrangements to come see him now, knowing that it might be her last chance but also that he might never know that she was there and that she might have to return soon after for a funeral. I told her to wait until we talked to the surgeon to get the last word.
Thursday Night
After what seemed like an interminable wait, the surgeon – who had been in surgery – finally arrived to give us the diagnosis and prognosis. He started by explaining that he had reviewed the records sent by Riddle, but had wanted to get all of his own tests so he could know all he needed. He then explained that Riddle had equipment that was limited in how it could detect certain aspects of my grandfather’s condition, and how the equipment that UPenn had was more advanced and had better detail. He then began to explain the situation in detail – which amounted to this: they were not going to operate, but NOT because of why we thought. Instead, it was because the situation wasn’t as serious as we had thought.
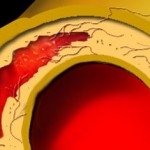 It turns out that the equipment at UPenn discovered that there was an aneurysm, but that it was only 5.2cm – well under the ‘terminal’ size (essentially, if your aorta is more than twice it’s normal size, it’s considered high risk, otherwise it’s treatable. So for a 3cm aorta, 6cm+ is extremely dangerous, but 5.2 was much more manageable). Moreover, it turns out that it wasn’t a classic aneurysm that runs the risk of rupture because the artery wall is torn (or dissected) – it was what is called a Intramural Hematoma (IMH)². Essentially, a smaller crack in the interior of the arterial wall allowed some blood get into the space between the inner and outer walls and created the aneurysm. The reason this isn’t as serious is because you have two essentially intact walls, which a) there is less risk of a rupture and b) there is less direct pressure from blood flow which can make the aneurysm grow.
It turns out that the equipment at UPenn discovered that there was an aneurysm, but that it was only 5.2cm – well under the ‘terminal’ size (essentially, if your aorta is more than twice it’s normal size, it’s considered high risk, otherwise it’s treatable. So for a 3cm aorta, 6cm+ is extremely dangerous, but 5.2 was much more manageable). Moreover, it turns out that it wasn’t a classic aneurysm that runs the risk of rupture because the artery wall is torn (or dissected) – it was what is called a Intramural Hematoma (IMH)². Essentially, a smaller crack in the interior of the arterial wall allowed some blood get into the space between the inner and outer walls and created the aneurysm. The reason this isn’t as serious is because you have two essentially intact walls, which a) there is less risk of a rupture and b) there is less direct pressure from blood flow which can make the aneurysm grow.
He said that surgery for this ran a 20-40% fatality rate, but that medicinal treatment to keep his blood pressure low until the small crack could heal and the hematoma could be reduced by the body should do the trick. It could still potentially kill him, and the artery would never fully recover at his age, but it wasn’t an immediate threat. Instead, he hoped that a 1-week stay would be sufficient to treat him. It was a long way from what we had been told up to then – aggravatingly so, to some degree – but in the end it was a much better result. Soon after, the calls went out: Grandpop was going to live.
Relief
The prognosis – while still serious -was a huge weight off of our shoulders. We all let out a collective sigh of relief and smiled. It had been a tumultuous 2 days, but it was all worth it in the end. Grandpop has been moved out of ICU to a private room, where he’ll stay for another 6 days, most of which he’ll probably spend sleeping as they keep his blood pressure unnaturally low to prevent any further damage. But even if he doesn’t speak, doesn’t get riled up like he’s prone to, it’s a bonus – he’s still around and will hopefully be around for some time yet.
¹Image from National Heart, Lung and Blood Institute
²Image from Radiology Assistant.nl
glad to hear your grandfather is doing well buddy. i know i’ve seen enough hospital rooms lately, we should gather for some beers some time.
Oh man, Marty. I know how tough the whole situation is, and it’s great that your family was able to come together to be near your grandpa when he needed you. I’m glad he’s out of the woods for now. Grandpas are wonderful things, and I hope yours is around for a good while longer.
I thought I left a comment here, but I guess not …
What an ordeal! That sounds incredibly stressful and draining, but I’m really glad the end result was better than expected. I hope he keeps holding on … like Sarah said, Grandpas are the best!